Robots and AI in Medicine: Revolutionizing Care or Replacing Jobs?
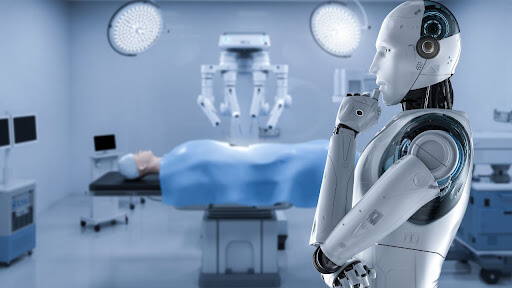
The rapid rise of robots and artificial intelligence (AI) has sparked intense debate about the future of work across industries, and the medical field is no exception. From science fiction visions of robotic surgeons to real-world AI diagnosing diseases, the question looms large: Are robots and AI going to take over all the jobs in the medical field in the future? This query taps into both hope and fear—hope for improved patient care, efficiency, and precision, and fear of job loss for millions of healthcare professionals. In this blog, we’ll explore the current role of robots and AI in healthcare, their potential to transform medical jobs, the tasks most at risk, the irreplaceable human elements, emerging opportunities, and the ethical and practical challenges ahead. Rather than a complete takeover, the evidence suggests a future of collaboration, where technology augments human expertise, reshapes roles, and creates new pathways in medicine.
The Current Landscape: Robots and AI in Healthcare Today
Robots and AI are already deeply embedded in the medical field, proving their value in diverse applications. The journey began in the 1980s with robots like the PUMA 560, which assisted in precision surgeries, marking a milestone in minimally invasive procedures. Today, the global medical robotics market, valued at $13.19 billion in 2023, is projected to grow to $52.41 billion by 2032 at a compound annual growth rate of 15.69%, with hospitals leading the charge. This growth reflects the expanding role of technology in healthcare.
Surgical robots, such as Intuitive’s da Vinci system, enhance precision in laparoscopic and robotic surgeries, reducing patient recovery time and surgeon fatigue. These systems process data from medical records and imaging to guide surgeons, minimizing human error. Beyond the operating room, autonomous mobile robots (AMRs) like Aethon’s TUG model transport supplies, laundry, and lab specimens, carrying up to 998 lbs (453 kg) across hospital departments using machine learning to navigate. Cleaning robots, such as Xenex’s UV disinfection models, sanitize spaces to curb infections, while social robots provide companionship and monitoring in long-term care settings.
AI, meanwhile, excels in data-heavy tasks. Algorithms analyze X-rays, MRIs, and CT scans, often detecting patterns—like early-stage lung cancer—with accuracy rivaling or surpassing human radiologists. A study cited by the American College of Surgeons noted a 5% higher detection rate for AI in certain cases. AI also streamlines administrative work: smart beds monitor vital signs and relay data to nurse stations, and generative AI, like that powering ChatGPT, organizes electronic health records (EHRs), summarizes patient histories, and reduces errors in documentation. In drug discovery, AI simulates scenarios and designs new candidates for clinical trials, accelerating innovation.
These advancements show robots and AI already complement healthcare workers, handling repetitive, logistical, and analytical tasks. But does this mean a full takeover of medical jobs is on the horizon? Let’s examine the potential.
Jobs at Risk: Where Robots and AI Might Dominate
Certain medical roles, particularly those involving repetitive, data-driven, or low-skill tasks, are vulnerable to automation. A 2019 report by Carl Benedikt Frey and Michael A. Osborne from the University of Oxford estimated that medical transcriptionists, health information technicians, and medical secretaries face a high likelihood of computerization, with physicians at a mere 0.42% risk. Here are the roles most susceptible:
1. Medical Transcriptionists: Speech recognition software now transcribes dictations from doctors into written reports with increasing accuracy, reducing the need for human transcribers.
2. Medical Coders and Billers: These professionals assign codes to procedures and diagnoses for insurance claims. AI algorithms perform this faster and more precisely, cutting costs and errors.
3. Medical Schedulers: Booking appointments and managing schedules can be handled by AI, which optimizes calendars and handles patient inquiries via chatbots.
4. Pharmacy Technicians: Robots like PharmaAssist dispense medications and track prescriptions, executing these tasks with efficiency and accuracy.
5. Medical Laboratory Assistants: AI can prepare and analyze patient samples for testing, often outperforming humans in speed and consistency.
6. Diagnostic Support Roles: In radiology and pathology, AI’s pattern recognition excels at reading scans and tissue samples, sometimes spotting anomalies humans miss.
The Health Foundation’s research found no single healthcare occupation can be fully automated, but tasks within these roles—especially repetitive or data-intensive ones—are prime targets. Automation aims to reduce overhead by cutting salaries, benefits, and human error, a key driver of robotic process automation (RPA) running 24/7. Posts on X and predictions from consultants suggest roles like medical records management and basic diagnostics could see significant AI infiltration within a decade. If costs for workload automation (ranging from $30,000 to $250,000 depending on IT complexity) drop, smaller clinics could adopt these tools, amplifying the shift.
Does this signal the end of human jobs in medicine? Not quite. While these tasks may vanish, the broader picture reveals limits to automation and a vital role for humans.
The Human Edge: Why Robots and AI Won’t Take Over Everything
Despite their prowess, robots and AI lack qualities intrinsic to human healthcare professionals, ensuring certain roles and tasks remain irreplaceable. Here’s why a complete takeover is unlikely:
1. Empathy and Compassion: Patients face vulnerability—fear of symptoms, anxiety over results, or the weight of a life-altering diagnosis. Doctors and nurses offer comfort, hold hands, and provide emotional support, building trust no algorithm can replicate. The human touch is central to the patient-centered model of care, rooted in compassion.
2. Complex Decision-Making: Medicine is nonlinear. Diagnoses and treatment plans aren’t always formulaic; they require creativity, problem-solving, and intuition. A doctor considers a patient’s lifestyle, emotional state, and unique history—nuances AI struggles to grasp. As Humanitas University notes, no algorithm can fully navigate these variables.
3. Social and Emotional Intelligence: Nurses and physicians communicate effectively, empathize, and adapt to diverse patients. A 2019 Office for National Statistics analysis ranked medical practitioners among the least automatable jobs, citing terms like “patient” and “treatment” in task descriptions.
4. Surgical Dexterity and Judgment: While robots assist in surgery, they can’t fully replace surgeons. Procedures are unpredictable—tissues vary, complications arise. Surgeons adapt in real time, a flexibility AI lacks. Even Elon Musk, in a 2025 X post, noted robots surpassed human precision for Neuralink’s brain-chip insertions, but human oversight remains critical.
5. Ethics and Accountability: Who’s liable for an AI error that costs a life—the creator, user, or machine? This ethical dilemma, highlighted by Keragon, underscores the need for human judgment. Patients also distrust life-or-death decisions by robots, as seen in an NHS chatbot trial where users preferred human appointments.
A 2021 Pew survey showed 77% of Americans support brain chips for paralysis but 56% oppose cognitive enhancement, reflecting a preference for human-led care. The American Medical Association echoes this, stating physicians using AI will outpace those who don’t, not that AI will replace them. Robots and AI excel in stable, predictable tasks, but medicine’s complexity demands human expertise.
A Collaborative Future: Augmentation, Not Replacement
Rather than a takeover, the future of robots and AI in medicine points to collaboration. Technology augments healthcare professionals, enhancing efficiency and outcomes while preserving the human element. Consider these examples:
1. Surgical Support: Robots like Intuitive’s Ion platform aid minimally invasive biopsies for lung cancer, guiding surgeons with precision. AI anticipates surgical steps, as seen in laparoscopic cholecystectomy studies, allowing real-time adjustments.
2. Diagnostics: AI speeds up scan analysis—X-rays, MRIs, CTs—flagging issues for radiologists to review. Oncology benefits from early cancer detection, with AI sometimes outperforming humans by 5%, but doctors verify and contextualize results.
3. Administrative Relief: Generative AI manages EHRs, summarizes notes, and schedules appointments, cutting the time doctors spend on paperwork (half their day, per one study). This frees them for patient care, reducing burnout and boosting job satisfaction.
4. Telehealth and Virtual Care: AI-powered virtual nurses and physicians handle preliminary screenings, asking standardized questions and compiling data from sensors. Remote monitoring via wearables aids chronic conditions like diabetes, with human clinicians overseeing complex cases.
5. Patient Experience: Robots deliver supplies, clean rooms, and guide visitors, while AI chatbots answer basic queries. This streamlines workflows, letting nurses and doctors focus on bedside care, improving patient comfort and engagement.
The NHS Long Term Workforce Plan and the 2019 Topol Review envision AI “augmenting rather than replacing” staff, giving clinicians “the gift of time.” A 2023 Health Foundation poll found 45% of healthcare workers see AI’s impact as positive, rising among those familiar with tech. Robots and AI handle mundane tasks—logistics, data entry—while humans tackle nuanced, interpersonal ones. This synergy, as Intel notes, leverages AI, computer vision, and edge computing to streamline workflows and improve outcomes.
New Opportunities: Jobs in the Age of AI
Far from eliminating jobs, robots and AI are poised to create new roles in healthcare, blending tech and medicine. The fear of mass displacement, voiced by some on X and in a PricewaterhouseCoopers report predicting 7 million job losses across industries, overlooks this potential. Here are emerging opportunities:
1. Chief AI Officer: Hospitals like the Mayo Clinic and UC San Diego Health are appointing doctors to oversee AI implementation, ensuring systems align with clinical needs and ethics.
2. AI-Enhanced Specialties: New subspecialties focus on data-driven medicine, using AI for diagnostics and treatment planning. Clinicians trained in AI will lead this shift.
3. Health Tech Implementation Specialists: These experts, akin to product managers, help integrate AI tools and proprietary platforms, bridging tech and healthcare.
4. AI Literacy Trainers: Educators teach healthcare workers to use AI, offering workshops on machine learning, data analysis, and practical applications.
5. Ethical AI Specialists: Professionals address bias in AI models, a concern amplified in healthcare where women and minorities face misdiagnosis risks due to underrepresentation in data. They ensure fair, transparent outcomes.
McKinsey and Harvard estimate AI could save the U.S. healthcare system $360 billion over five years by optimizing processes. Workers with skills in Python, R, SQL, and healthcare standards (HL7, FHIR) will thrive, as will those collaborating across disciplines. Amazon’s “Upskilling 2025” program, investing $1.2 billion to retrain 300,000 employees, shows how retraining can prepare workers for tech-driven roles. Rather than replacement, AI redirects human effort to complex, rewarding tasks, potentially shortening workweeks, though pay and benefit impacts remain unclear.
Challenges and Considerations
A full takeover by robots and AI faces significant hurdles, tempering the pace of change:
1. Cost: Initial investments in robots, AI systems, and training are steep—$30,000 to $250,000 for automation solutions. Maintenance and updates add to the burden, limiting adoption by smaller facilities.
2. Integration: Seamless workflow integration requires interoperability with EHRs and real-time data access. In surgery, responsiveness is critical for safety.
3. Safety: Human-robot interaction risks system failures with dire consequences. Rigorous testing and protocols are needed to minimize harm.
4. Ethics and Bias: AI can amplify biases in training data, misdiagnosing underrepresented groups. Continuous monitoring and ethical guardrails are essential.
5. Public Trust: A 2023 Pew survey found 60% of Americans are uncomfortable with AI-driven care, preferring human providers for empathy and accountability.
6. Job Displacement: While not all jobs vanish, repetitive roles face risk. Retraining is key, but not everyone can adapt, raising economic concerns.
Experts like Brigette Hyacinth and panelists at the 2017 Canadian Agency for Drugs and Technologies in Health Symposium argue AI won’t replace humans but enhance decision-making. The industrial revolution augmented humans; AI risks replacing some, but the human touch—empathy, creativity—remains vital.
The Verdict: Collaboration, Not Conquest
Are robots and AI going to take over all medical field jobs in the future? The evidence says no. While repetitive, data-driven tasks—transcription, coding, scheduling—face automation, the core of healthcare resists a full takeover. Empathy, complex judgment, and the art of patient care demand human presence. Robots assist in surgery, deliver supplies, and sanitize rooms; AI excels in diagnostics, record management, and drug discovery. Together, they free clinicians from busywork, reduce burnout, and improve outcomes.
The future is collaborative: technology amplifies human skills, not replaces them. New roles—AI officers, tech specialists, ethicists—emerge, requiring retraining and adaptability. Challenges like cost, safety, and bias persist, but with responsible integration, robots and AI can revolutionize medicine without sidelining its human heart. Doctors, nurses, and patients will navigate this era together, blending precision with compassion for a healthier tomorrow.

No comments: